Drawing and Neurosurgery – how far apart are these two different worlds?
I have always been interested in art. It is magical how art can convert an idea or emotion that is hidden inside your brain into something that other people can see, or even touch. In this way, drawing became not only a hobby, but also a way to “talk” and connect to people. When I was a kid, growing up in Ourinhos, Brazil, my parents would say that my favorite toys were a pencil and a piece of paper (Figure 1).
Figure 1. The author, in 1995, drawing circles and lines on a piece of paper - the beginning of a passion. Ourinhos, Brazil.
Over the years, I developed my own drawing style, mostly inspired by realistic sketches. Playing with shadows and lights using a grey or black-toned palette captivated me (Figure 2). The simple tools (a piece of paper and a pen or pencil) made it a very accessible leisure. Today, each drawing takes me hours to complete, yet I always enjoy keeping the sketches over my desk, so I can add or remove details, almost turning them into experiments and analyzing the results over time.
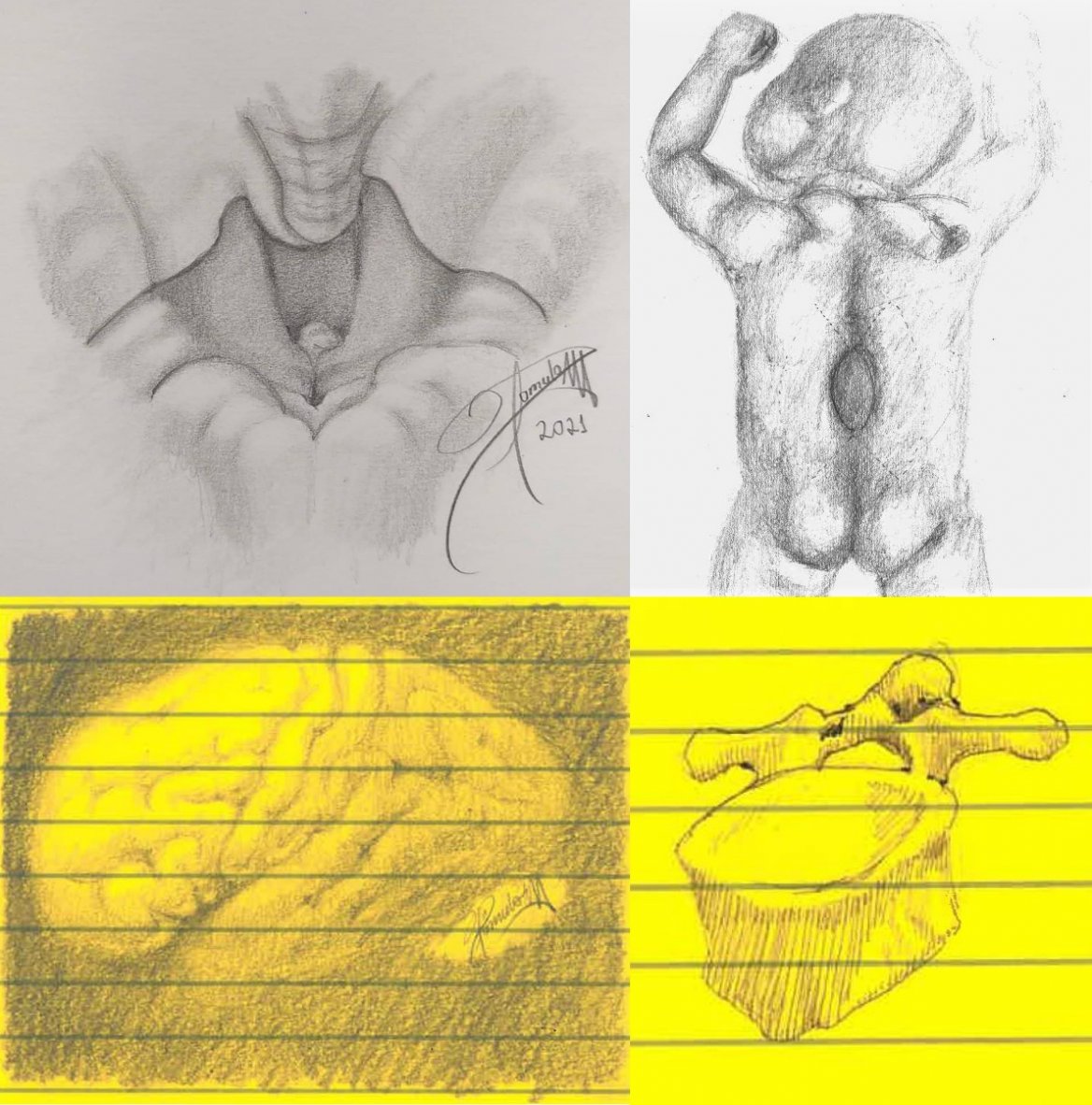
Figure 2. The greyscale sketches have always caught my attention, becoming my main drawing style: fourth ventricle with the tela choroidea removed, posterior-inferior view (top left); myelomeningocele with skin marks planned for helping the closure of the defect (top right); brain, lateral view (bottom left); thoracic vertebra (bottom right).
I have also found drawing to be a useful tool in life - during the intense studying periods of college and medical school, I benefited from converting extensive texts into a simple picture that could show key ideas in an easy-to-remember way. I really enjoyed spending time using my hands to create and transform - Sketching on paper or, more recently, using a computer painting software (Figure 3). This taste for manual work led me to pursue a career in surgery.
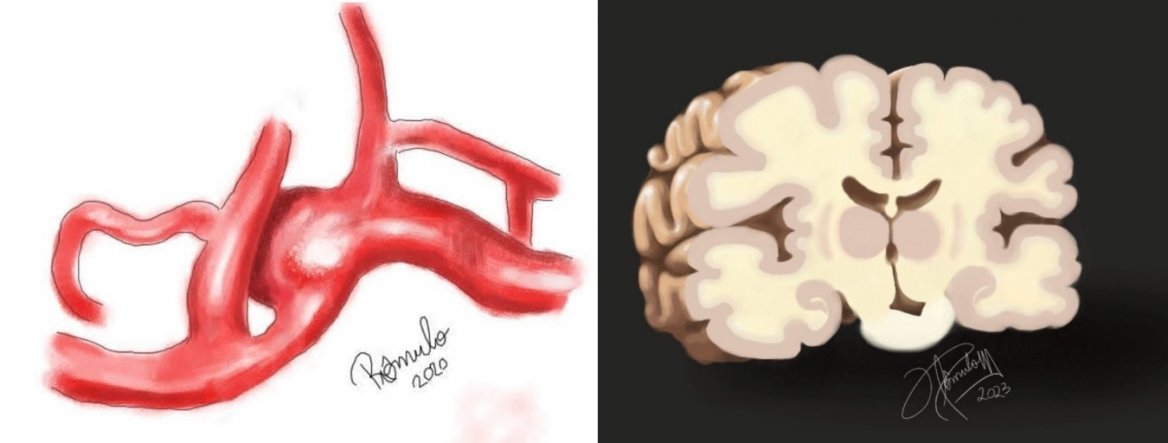
Figure 3. In the last few years, I have included modern drawing software in my art toolkit. On the left, an anterior communicating artery aneurysm. This drawing was based on a real angiographic study and helped our team to plan the surgical approach and clip position. On the right, a coronal section of the brain.
In many ways, drawing also accompanied me throughout neurosurgery training. I created sketches of the patient’s anatomy and pathology, so I could simulate and plan the best approach to the disease. Then, by the time of the real operation, I would have already performed the procedure a few times over in my head and on paper, so I was more prepared and confident. Drawing also helped me communicate. They enriched discussions with my mentors and facilitated teaching to patients or younger residents. The phrase “a picture is worth a thousand words” proved to be true in many situations. I even had the opportunity to draw, with the aid of friends, a logo for our neurosurgery program, in Campinas, Brazil, for which I am very proud of (Figure 4).
Figure 4. The logo of the neurosurgery residency program from the Universidade Estadual de Campinas (Unicamp), Campinas, Brazil.
I do think that art and neurosurgery have more in common than one might think. The nervous system itself is nature’s multidimensional masterpiece: high specialized neurons arranged in layers and scaffolded by glial cells, forming an amazing structure where architecture and functionality intermingle. In addition, the drawing process reminds me of the operations themselves. The delicate pencil strokes are, for example, like the blade or scissors moving in the opening of the arachnoid bands of the brain’s fissures. When drawing, you start with a blank paper piece and a pencil. By adding layers over layers of dark graphite, a recognizable image starts to form. The artist must be aware of the pencil’s pressure over the paper, the amplitude of movement and the condition of the instruments. The artist must have in mind what the final product should look like, which allows the precise reproduction of what he or he sees or intends to create. In the operating room, something more complex, but similar, happens. The surgeon initially sees a nervous system distorted by a disease, the natural layers are displaced, and the patient is suffering. These layers are removed or split carefully one by one, and, with some time, the hidden normal structures reveal themselves, forming the beautiful normal anatomy of the human brain and spine. In this process, the work of each hand must be precise and coordinated, and each movement calculated in amplitude and power. It is the careful calibration of these movements that allow and experienced surgeon to achieve what is intended. Both unnecessary maneuvers and harm can be avoided. In the end, the artist and the surgeon are rewarded for their work with a new creation: a unique piece of art or a restored human body.
Throughout all our years of training, surgeons must develop certain skills to differentiate normal to abnormal tissue by the guidance of visual, tactile, and even auditory cues (Catalino, M.P., et al., 2022) – this is of special interest in cancer surgery when there is loss of distinct planes due to invasive disease. In this sense, artists may take advantage of their familiarity to color hues and textures. Furthermore, both drawing and surgery require tridimensional knowledge and spatial orientation that can be synergistically improved by their individual practice. I believe that my drawing helps me operate and operating helps me draw.
In conclusion, neurosurgery and drawing may look like completely different things at a first sight. However, with a closer look you can see striking similarities. The neurosurgeon who is also an artist may find in their art not only a simple hobby, but also a great ally to their medical career.
References
- Catalino MP, Buss E, Chamberlin G, Trembath D, Morgan D, Krebs M, Ewend MG, Jaikumar S. Tumor sound, auditory cues, and tissue pathology in glioma surgery: a proof-of-concept study. J Neurosurg. 2022 Dec 30:1-9. doi: 10.3171/2022.11.JNS222114. Epub ahead of print. PMID: 36585869.
The author:

Dr. Rômulo Augusto Andrade de Almeida, MD, was born in Brazil, in 1994. He achieved the medical graduation from Universidade Positivo, Curitiba, Brazil, in 2017, and became a neurosurgeon by the Universidade Estadual de Campinas, Campinas, Brazil, in 2023. Currently, he works as a researcher at the Neurosurgery Department of the MD Anderson Cancer Center, focusing on spine surgery and oncology research.